Story Highlight
– Dozens of deaths linked to weight loss jabs reported.
– 52 fatal reports for GLP-1 injections since 2024.
– Experts warn about inappropriate use among slimmer adults.
– Severe complications include gallstones and pancreatitis risks.
– Calls for stricter regulations on weight loss drug prescriptions.
Full Story
Dozens of fatalities among middle-aged individuals in the UK have been linked to popular weight loss injections, according to recent reports. The rise of drugs like Ozempic, Mounjaro, and Wegovy has seen health regulators record 52 deaths associated with GLP-1 injections since 2024. Medical professionals have raised concerns over the growing death toll, especially given the surge in people seeking these medications to address the nation’s obesity crisis.
Tam Fry, chair of the National Obesity Forum, stated that while these drugs can significantly aid those who genuinely need assistance with their weight, they are being misused by individuals who wish to simply shed a few pounds. “If you take them and you don’t need them, and you break the rules, you run the risk of serious complications – or death,” Fry cautioned. He expressed that many people assume adverse effects won’t happen to them, but the reality is that such risks are very much present.
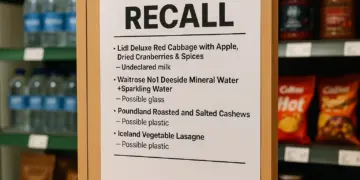
The Medicines and Healthcare products Regulatory Agency (MHRA), which oversees drug safety in the UK, reported a total of 173 fatal outcomes linked to GLP-1 injections. Side effects reported have also increased in tandem with the growing number of prescriptions, as the weight loss effects of these drugs have attracted attention in the fight against obesity. It is estimated that approximately 1.5 million people in the UK are using weight loss injections procured through private online pharmacies, with an additional 200,000 receiving prescriptions through the NHS.
However, there are rising concerns regarding their side effects. Mild reactions can include headaches, nausea, and gastrointestinal issues, but more severe complications such as gallstones, kidney stones, and inflammation of the pancreas have also been reported. A small number of fatalities connected to these weight loss injections involved younger adults; specifically, two individuals in their 20s were among the deceased. However, the majority of fatalities were middle-aged, with deaths recorded among those in their 30s (eight), 40s (15), and 50s (37).
It is crucial to note that a report submitted to the MHRA does not necessarily imply that the drug was the cause of death. The fatal incidents could be entirely coincidental. Factors such as pre-existing health conditions or interactions with other medications might have played a role. For instance, obesity itself is a significant contributor to conditions like cancer and heart disease, two of the UK’s leading causes of mortality.
Given the popularity of these medications, experts are concerned that the figures compiled by the MHRA may not represent the full extent of the issue. Many potential side effects go unreported; estimates suggest that only about one in ten serious adverse reactions are actually logged with the MHRA.
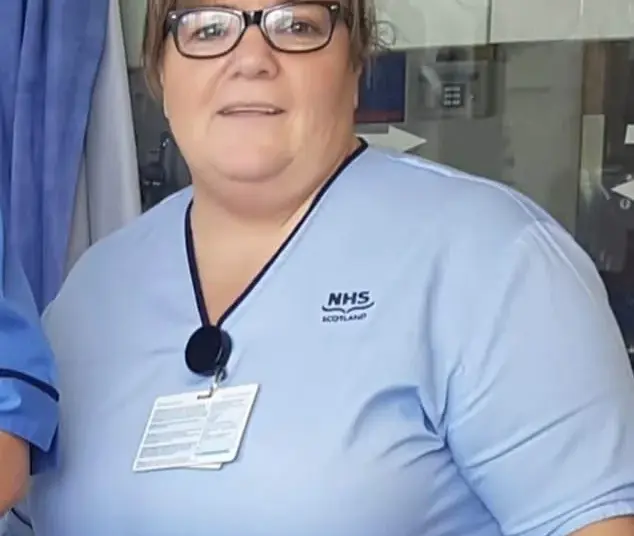
Last year, a case emerged that underscored the potential dangers of these drugs, involving a nurse from Scotland. Susan McGowan, aged 58, experienced multiple organ failure after taking Mounjaro, and her death was subsequently linked to the drug. She purchased the medication from an online pharmacy and succumbed to complications at University Hospital Monklands in Airdrie in September 2024. The causes recorded on her death certificate included multiple organ failure and septic shock, with the use of tirzepatide noted as a contributing factor.
The MHRA operates the Yellow Card scheme for monitoring drug safety, a system established after the thalidomide tragedy of the 1960s. This platform allows medical practitioners and patients to report adverse reactions to medications. Reports filed here may lead to deeper investigations and hopefully improve drug safety through regulatory action, including label warnings or drug withdrawals.
While all drugs available in the UK undergo comprehensive clinical trials before approval, some issues may arise post-market entry, similar to the rare blood clots associated with AstraZeneca’s COVID-19 vaccine. Newly introduced medications, including Ozempic and Mounjaro, are subject to additional scrutiny under a special monitoring scheme indicated by a Black Triangle symbol, highlighting the need for ongoing oversight.
An analysis indicated that exenatide, sold as Bydureon, was linked to 55 fatalities, making it the most concerning of the GLP-1 medications examined. It is typically prescribed solely for type 2 diabetes, which is similar to the prescribing guidelines for dulaglutide (Trulicity) and lixisenatide (Suliqua). Meanwhile, semaglutide, found in Ozempic and Wegovy, accounted for 31 deaths, while tirzepatide was linked to 38 fatalities.
The function of these injections is rooted in their ability to imitate a natural hormone known as glucagon-like peptide-1 (GLP-1), which is secreted by the gut upon eating. This hormone enhances insulin production, reduces glucose output from the liver, slows digestion, and can suppress appetite.
Amid reports of misuse, medical professionals are calling for stricter regulations concerning the prescription of these weight loss treatments. Fry commented on the challenge: “The problem is that they work; the genie is out of the bottle”. With the rise in popularity associated with celebrity endorsements, many have sought these medications without proper medical guidance. High-profile figures like Kim Kardashian have contributed to this trend, as have cases like that of model Lottie Moss, who suffered severe health complications after using Ozempic.
Health authorities caution that the use of these medications should be strictly restricted to individuals suffering from obesity or related illnesses, administered only under professional supervision.
While politicians have generally welcomed the introduction of these medications, citing their potential economic benefits, the MHRA and health officials continue to stress the importance of regulated use. The Department of Health has reiterated that weight loss drugs must be viewed as part of a broader strategy, not as quick fixes for simple weight concerns.
Dr Alison Cave, Chief Safety Officer at the MHRA, reaffirmed their commitment to safety monitoring, stating, “We continually monitor the safety of medicines… and act promptly to address any identified risks.” She highlighted the significance of consultation with healthcare professionals regarding the potential side effects associated with GLP-1 medications.
In summary, while GLP-1 injectables present opportunities for effective weight management, the associated health risks—especially concerning inappropriate use—prompt critical scrutiny and call for ongoing dialogue between healthcare providers, regulatory bodies, and patients.
Our Thoughts
To mitigate the fatalities linked to GLP-1 weight loss injections, strict regulatory compliance and supervision are essential. The misuse of these medications by individuals who do not meet the criteria for prescription is a critical issue. Under the Medicines Act 1968 and the Misuse of Drugs Regulations, there should be rigorous enforcement to prevent unauthorized access to these drugs through online pharmacies.
Key safety lessons include the necessity for comprehensive patient education on the appropriate use of these medications and the potential risks of misuse. Enhanced monitoring and reporting systems could ensure more incidents are documented accurately, promoting safer use. Furthermore, greater collaboration between healthcare providers and regulatory bodies could facilitate real-time data sharing regarding adverse effects, thereby improving drug safety protocols.
Failing to meet safety and monitoring regulations could constitute a breach of the Health and Safety at Work Act 1974. To prevent similar incidents, it is crucial to implement stricter criteria for prescribing these drugs, enforce penalties for fraudulent procurement, and increase awareness campaigns regarding the dangers of unsupervised usage of weight loss medications.




















These reports are deeply concerning. Medications that alter metabolism and appetite can have serious side effects and must be prescribed and monitored by qualified clinicians. Using GLP1 drugs without medical need or oversight increases the risk of complications such as pancreatitis and gallbladder disease. Regulators and prescribers should tighten controls, ensure clear guidance on eligibility and duration of treatment, and improve public education so people understand both benefits and risks.
This is deeply worrying. These medications can offer real benefits when prescribed and monitored properly but they are not without serious risks. Misuse by people seeking quick weight loss and inadequate oversight can lead to severe complications and even death. Stronger regulation, better public information about risks and safer prescribing practices are needed now to protect patients.
These reports are deeply concerning. GLP 1 drugs can be effective when prescribed and monitored for people with appropriate medical indications but they are not without serious risks. Misuse by people seeking quick weight loss, off label use, and inadequate clinical oversight increase the chance of complications such as pancreatitis and gallbladder disease and can lead to fatal outcomes. Stronger regulation on prescribing and supply, better patient education about risks and signs of complications, and ensuring access to multidisciplinary care for weight management would help protect patients while allowing safe, evidence based use of these medicines.