Story Highlight
– Fat jabs help over a million Brits lose weight.
– Rise in haemorrhoids linked to GLP-1 weight loss drugs.
– Constipation from fat jabs causes discomfort and complications.
– Health expert reports 41% increase in haemorrhoid cases.
– Patients advised to maintain hydration and fiber intake.
Full Story
For a significant number of individuals in the UK, weight loss injections, often referred to colloquially as “fat jabs,” have led to remarkable transformations in their battle against obesity. These medications are credited with diminishing hunger levels, reducing the incessant cravings for food, and enabling users to shed unwanted pounds effectively.
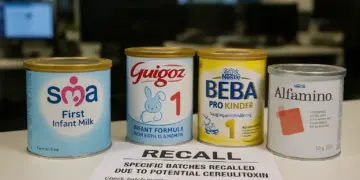
However, while the benefits can be transformative, a growing number of users are also reporting unexpected side effects—one of which is both uncomfortable and, for many, quite embarrassing. Recent observations from healthcare professionals indicate an increase in cases of haemorrhoids among individuals utilising GLP-1 (glucagon-like peptide-1) receptor agonists, which include popular drugs like Mounjaro and Ozempic.
Dr. Ross Perry, who serves as the medical director of Cosmedics Skin Clinics, has noted a concerning trend in his practice. “Over the past year, we have witnessed a 41% increase in patients diagnosed with haemorrhoids, many of whom are taking GLP-1 drugs for weight management,” he stated. This rise in occurrences appears to correlate with the increasing popularity of these medications.
Haemorrhoids, commonly known as piles, occur when veins in the anal canal swell, causing symptoms such as itchiness, pain, and swelling. A key contributor to this condition is constipation, which has been frequently reported by those undergoing treatment with these weight loss medications. Dr. Perry elaborated further: “Many of our patients report significant changes in bowel habits after starting these drugs, and the associated constipation often leads to the development of haemorrhoids.”
As patients increasingly turn to physical exercise to combat muscle loss associated with weight reduction, they may inadvertently exacerbate their symptoms. Engaging in weight training can lead to straining during bowel movements, creating a cycle that worsens the condition.
The NHS defines haemorrhoids as lumps that can form around the anal area, which can cause various symptoms, including bright red blood during bowel movements, persistent itching, and a sensation of incomplete bowel evacuation. The delayed gastric emptying induced by GLP-1 medications plays a pivotal role in this issue, creating drier and harder stools. Dr. Perry explained, “The slow gut motility caused by these medications can make it difficult for patients to pass stools comfortably, leading to straining that causes piles, along with potential small tears and anal skin tags.”
Several individuals have shared their experiences online, highlighting the unpleasant realities accompanying their weight loss journeys. One 59-year-old woman recounted her journey on Ozempic, where she lost 40 pounds in six months. However, her excitement was tempered by the development of haemorrhoids, which her gastroenterologist attributed directly to the chronic constipation caused by the medication. Another individual reported similar digestive issues even when taking lower doses of weight loss drugs, leading them to rely on daily stool softeners for relief.
While for many, the symptoms of haemorrhoids may resolve spontaneously within a few days, there are instances where discomfort escalates. Dr. Perry asserts that patients often wait until their pain becomes unmanageable before seeking medical attention. “It’s not uncommon for patients to endure significant discomfort for extended periods, only to eventually seek help when they can no longer tolerate the pain,” he noted.
Individuals experiencing symptoms related to haemorrhoids are advised to consult their general practitioners initially. The NHS recommends a diet rich in fibre and adequate hydration as essential measures to alleviate constipation. Adults should aim for approximately 30g of fibre per day, a target many find challenging to meet. Incorporating foods such as porridge, wholemeal bread, and various fruits and vegetables can significantly improve one’s fibre intake.
In addition to dietary changes, healthcare professionals recommend reducing caffeine and alcohol consumption, as both can exacerbate haemorrhoid symptoms. Various techniques, like using moist toilet tissue and applying ice packs wrapped in cloth to swollen areas, may offer temporary relief. For persistent cases, GPs often initiate treatment strategies that focus on dietary adjustments, the use of over-the-counter remedies, or recommend prescribed creams.
When conservative treatments are ineffective, referrals to specialist colorectal teams may become necessary. Dr. Perry’s clinic also offers innovative treatments for severe cases of haemorrhoids, including a minimally invasive procedure employing radiofrequency technology known as The Rafaelo, which aims to shrink and eliminate haemorrhoidal tissue.
Despite the potential issues associated with haemorrhoids, many individuals remain focused on the substantial benefits they have realised from weight loss injections. Leading pharmaceutical companies involved in producing GLP-1 medications, such as Novo Nordisk, assert their commitment to patient safety and urge users to report side effects. A spokesperson emphasised the importance of using these medications under the guidance of healthcare professionals and indicated that ongoing safety data collection is a priority.
It remains critical for patients to be aware of concerning symptoms signalling a need for medical intervention. Notably, symptoms that overlap with serious conditions, including bowel cancer, must not be overlooked. Warning signs such as persisting rectal bleeding, drastic changes in bowel habits, unexplained weight loss, and abdominal discomfort necessitate prompt medical review.
Dr. Perry cautioned against assuming that all rectal bleeding is attributable to haemorrhoids. “Anyone experiencing unresolving rectal bleeding must consult their GP, as it may indicate a more serious underlying issue,” he stated. Regular screenings and awareness of bodily changes can be paramount in ensuring overall health and wellbeing during weight loss journeys.
Our Thoughts
The article indicates a rise in haemorrhoids among users of GLP-1 weight loss drugs, correlating with increased constipation linked to these medications. To mitigate such complications, several preventive measures and regulatory considerations are essential.
Firstly, proper patient education regarding potential side effects and the importance of dietary adjustments is crucial. Users should be informed about maintaining adequate hydration and fibre intake to counteract constipation, thereby reducing the risk of haemorrhoids. This aligns with the Health and Safety at Work Act 1974, which mandates that employers provide necessary information for patients regarding the safe use of medications.
Additionally, healthcare professionals should adopt a more rigorous monitoring system for patients on GLP-1 drugs, ensuring that any adverse effects are promptly reported and addressed. This can prevent the escalation of side effects and enhance patient safety.
Finally, there may be implications for regulatory compliance if manufacturers are not effectively communicating risk management concerning these medications. Enhanced oversight from regulatory bodies, such as the MHRA, could further prevent similar incidents by ensuring that all side effects are transparently reported and managed.



















Constipation is a known side effect of many medications and can increase the risk of haemorrhoids, so it is sensible to remind people using GLP 1 treatments to monitor their bowel habits and take simple measures such as increasing dietary fibre and fluid intake. Employers and clinics offering these treatments should ensure patients receive clear advice about managing common side effects and know when to seek medical help, and workplaces should consider access to appropriate welfare facilities for staff undergoing treatment.
Important to highlight that any new medicine can have side effects and employers and workers should be aware of potential impacts on wellbeing and performance. Constipation and related conditions can be distressing and may affect attendance and concentration at work. Encouraging people to follow medical advice on diet fluid intake and reporting symptoms early is sensible. Occupational health services and managers should ensure staff using these medications have access to guidance and reasonable adjustments where needed.
Important to raise awareness that rapid weight loss and medications affecting digestion can cause constipation which in turn may lead to or worsen haemorrhoids. Employers and safety teams should ensure staff using these treatments know simple preventative steps such as increasing fibre and fluids, using stool softeners if advised by a clinician, and seeking prompt medical advice for persistent symptoms. Occupational health services can support education and reasonable adjustments for anyone experiencing pain or discomfort at work.
Important to acknowledge patient experiences while focusing on practical prevention. Constipation is a known side effect of GLP 1 drugs and can contribute to haemorrhoids through strain. Employers and safety professionals should encourage people using these medications to review side effects with their clinician and consider workplace adjustments such as access to drinking water, regular breaks to move and use the toilet, and information about dietary fiber. Clear communication about risks and simple mitigation measures can reduce discomfort and avoid unnecessary embarrassment.