Story Highlight
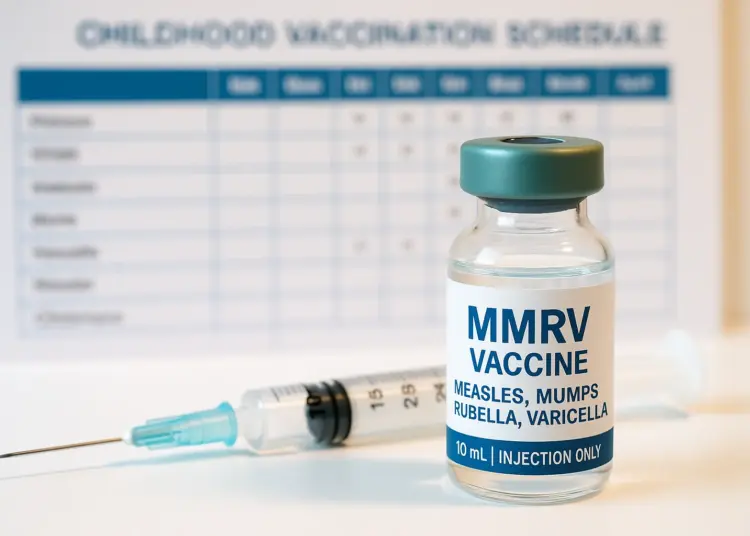
– NHS adds chickenpox vaccine to childhood MMR program.
– MMRV vaccine protects against measles, mumps, rubella, chickenpox.
– Historic milestone for children’s health, says Health Secretary.
– Rollout to begin for hundreds of thousands of children.
– Parents encouraged to vaccinate for serious chickenpox risks.
Full Story
From January 2, 2026, the NHS has launched an important initiative to protect children’s health by introducing a vaccine for chickenpox as part of a combined MMRV immunisation. This development will see the childhood vaccination programme expanded to include a safeguard against the varicella zoster virus, which is responsible for chickenpox.
Health Secretary Wes Streeting heralded the introduction of this vaccine as a significant advancement in public health. “Today marks a historic milestone in protecting our children’s health. For the first time, the NHS is offering chickenpox vaccination as part of our routine childhood immunisation programme,” he noted. This new addition comes in response to concerns about the impact of chickenpox on families, noting that the illness can lead to serious complications in some cases, as well as disruption to schooling and parental responsibilities when children are unwell at home.
The decision to incorporate the chickenpox vaccine came from the Joint Committee on Vaccination and Immunisation (JCVI), which made this recommendation in 2023. The JCVI’s findings were accepted by the UK and devolved governments, allowing the NHS to roll out the vaccine programme across England, Scotland, Wales, and Northern Ireland. With this rollout, hundreds of thousands of children will be eligible for the new combined MMRV vaccine.
Local healthcare providers will contact parents with children in the eligible age range, as the incorporation of the chickenpox vaccine means that many young individuals will receive the new combined jab during their routine vaccinations. Dr Gayatri Amirthalingam, who serves as the deputy director of immunisation at the UK Health Security Agency, expressed optimism about the effectiveness of the new vaccine. “Most parents probably consider chickenpox to be a common and mild illness, but for some babies, young children and even adults, chickenpox can be very serious, leading to hospital admission and tragically, while rare, it can be fatal,” she explained. She further emphasised that this vaccine has a proven track record of safety and effectiveness in countries that have used it for many years.
Historically, parents concerned about chickenpox had to seek private vaccination services, typically incurring a cost of around £150 per child. The NHS only previously provided vaccines to children deemed at high risk, such as those who had close contacts with immunocompromised individuals. The new MMRV vaccine aims to afford widespread protection, addressing both health concerns and the inconvenience of chickenpox outbreaks.
Chickenpox often causes mild illness in most children, with symptoms such as an itchy rash, fever, and fatigue. However, complications can arise, including bacterial infections, neurological issues such as encephalitis, lung infections, and, in very rare cases, death. Infants under four weeks of age and adults are particularly vulnerable to severe illness resulting from chickenpox.
The NHS plans to offer this vaccine in a structured manner. Children born on or after January 1, 2025, will receive their first and second doses at 12 and 18 months, respectively. For those born between July 1, 2024, and December 31, 2024, doses will be administered at 18 months and then again at three years and four months. This rollout also includes a catch-up programme for children born between January 1, 2020, and August 31, 2022, to ensure that those who may have missed earlier vaccinations can receive them.
There has been considerable support for this initiative among healthcare professionals. Professor Steven Turner, President of the Royal College of Paediatrics and Child Health, welcomed the news, highlighting that vaccinations are a crucial method for safeguarding children’s health and preventing severe illness. “Making sure your child is vaccinated is a vital step for parents and carers in keeping them safe,” he stated.
The integration of the chickenpox vaccine into the childhood immunisation schedule is poised to considerably enhance public health initiatives in the UK. As chickenpox is both a widespread and at times disruptive infection, parents can take comfort in knowing that their children will soon have access to better protection against this illness. The availability of MMRV as part of the routine vaccination programme not only presents an opportunity to increase immunity within the population but also aims to reduce the number of hospitalisations and serious illness linked to chickenpox.
As the rollout progresses, it is anticipated that greater awareness and participation among parents and guardians will lead to a higher uptake of the vaccine. The NHS’s commitment to enhancing children’s health through effective vaccination programmes is a vital part of broader public health strategies aimed at promoting wellbeing across society. The adoption of the combined MMRV vaccine into the existing framework illustrates a proactive approach in tackling common childhood diseases, enabling families to focus on health and development without the added worry of preventable illnesses like chickenpox.
Our Thoughts
The rollout of the combined MMRV vaccine against chickenpox marks a significant step in public health for childhood immunisation in the UK. To enhance safety and effectiveness, several preventive measures and lessons can be highlighted:
1. **Awareness and Education**: Prior to introduction, increasing awareness among parents about the severity of chickenpox could have alleviated misconceptions regarding its mildness, potentially improving vaccination uptake before rollout.
2. **Regulatory Compliance**: Adhering to the Health and Safety at Work Act 1974 mandates ensuring the safety and welfare of the public. Engaging communities earlier with information sessions could better inform parents about vaccinations, leading to higher compliance.
3. **Monitoring and Reporting**: Establishing strong post-vaccination monitoring systems in line with the MHRA regulations could help identify and respond to any adverse reactions quickly, ensuring public trust in the vaccine.
4. **Accessibility and Inclusivity**: Making the vaccine available to all socio-economic groups was crucial. Ensuring equitable access must remain a priority to avoid health disparities.
5. **Preventive Protocols**: Following recommendations from the NHS and JCVI, maintaining routine vaccination schedules, and offering catch-up programmes helps mitigate the risk of outbreaks and community spread.
Implementing these measures can enhance the effectiveness of vaccination programs and prevent similar issues in the future.