Story Highlight
– NHS incurs up to £20,000 per patient for complications.
– Six Britons died in Turkey from surgical procedures.
– Majority of patients seeking surgery abroad are female.
– Study highlights risk of serious post-operative complications.
– Government plans to enhance safety measures for medical tourism.
Full Story
The National Health Service (NHS) is incurring significant costs due to complications arising from cosmetic and obesity surgeries carried out abroad, with expenses reaching as high as £20,000 per patient. This troubling trend has been particularly highlighted in the context of surgical tourism, which has seen an alarming rise in patients seeking procedures in countries such as Turkey. Recent statistics indicate that the NHS is now faced with the aftermath of these surgeries, which often result in serious health risks, including instances of infection and the need for prolonged hospital care.
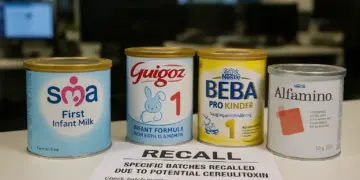
A comprehensive study published in BMJ Open has revealed that a growing number of patients returning to the UK require extensive treatment for complications linked to surgeries performed in foreign clinics. Procedures commonly sought include bariatric surgery, breast augmentation, tummy tucks, and other cosmetic enhancements. Disturbingly, reports detail that there have been at least a dozen fatalities associated with these surgeries, with six British citizens reported to have died in Turkey in 2024 alone, following medical operations.
The analysis conducted by researchers from Cardiff and Bangor universities reviewed data collected from 37 separate studies, focusing on patients who were admitted to the NHS due to complications linked to laparoscopic and aesthetic surgeries performed outside the UK. The majority of these patients—approximately 90%—were women, with an average age of 38. Turkey emerged as a predominant destination for these medical procedures, accounting for 61% of surgeries sought abroad.
Financially, the burden on the NHS has been substantial, with each patient requiring intervention costing between £1,058 and £19,549. However, the researchers have cautioned that these figures may still not fully represent the total financial impact, as they do not include costs associated with subsequent GP appointments, nursing care, and other medical necessities after the initial hospital stay. Notably, some patients have endured extensive hospital admissions, some lasting up to 49 days, which underscores the severity of the complications faced.
The researchers’ findings reveal a concerning pattern. Among the 371 patients assessed more closely, over half (53%) encountered moderate to severe complications post-surgery. These complications included severe infections necessitating intensive care and extensive antibiotic treatments. Alarmingly, there have been cases of multiple organ failure and other critical health issues arising from post-operative infections, leading to significant morbidity and mortality, including hypoxic brain injuries and cardiac incidents.
The study calls for increased awareness among potential patients considering surgical options abroad. The authors state that many individuals are unaware of the risks and the potential financial implications if they encounter complications once back in the UK. The NHS is often forced to provide emergency care without complete medical records or detailed information about the procedures undertaken overseas, complicating the treatment process for health professionals.
In response to these issues, the researchers and various healthcare professionals have advocated for public health campaigns aimed at educating individuals about the possible ramifications of undergoing medical procedures abroad. Professor Vivien Lees, vice-president of the Royal College of Surgeons of England, highlighted the dilemma faced by patients, who are often tempted by the allure of lower costs and attractive marketing from foreign clinics. She expressed concern that the NHS is unduly burdened with managing the fallout from decisions made by patients seeking cheaper options.
The calls for action have been echoed by the UK’s Secretary of State for Health, Wes Streeting. Following a series of tragic outcomes linked to cosmetic surgeries abroad, he urged caution for those considering such treatments, highlighting the risks associated with deals that appear excessively cheap. Streeting stated that while the NHS would never turn away individuals in need of care, the added burden of treating complications from international surgeries is an unwelcome strain on the already stretched health service.
Recent cases of adverse outcomes from foreign cosmetic surgeries have struck a chord in the public consciousness. For instance, Kaydell Brown, 38, from Sheffield, tragically passed away after undergoing multiple surgeries in Turkey, while others have suffered serious complications that led to their demise following procedures such as Brazilian butt lifts and gastric sleeve surgeries. These tragedies have sparked further scrutiny on the standards of care in private clinics abroad and the responsibilities that come with choosing to undergo such procedures.
The Department of Health and Social Care reiterated its concern regarding the trend of medical tourism, emphasizing ongoing efforts to clamp down on unsafe practices and raise awareness of the potential risks associated with international medical care. By engaging actively with overseas governments, they aim to enhance the safety and information available to patients contemplating treatments abroad, reaffirming a commitment to protect the health and well-being of UK citizens.
As the phenomenon of surgical tourism continues to grow, there is an urgent need for informed choice and protective measures for those seeking medical interventions beyond UK shores. The interplay between cost, regulatory challenges, and patient safety remains a pressing public health issue. Building on existing initiatives, it is crucial that more comprehensive data collection and public information campaigns be designed to safeguard individuals against the potentially devastating consequences of inadequate medical care abroad.
Our Thoughts
To mitigate the risks associated with cosmetic and obesity surgeries abroad, key interventions could include rigorous pre-operative assessments and comprehensive patient education to inform potential patients of the risks and costs of surgeries performed overseas.
The NHS is facing significant strain due to complications arising from these procedures, suggesting a breach of the duty of care expected from healthcare providers abroad. Relevant UK regulations include the Health and Safety at Work Act 1974, which emphasizes the duty to protect individuals from risks. Adequate aftercare protocols should also be established by overseas providers to ensure patients receive proper follow-up care, thus reducing post-operative complications.
Furthermore, public awareness campaigns should be implemented to caution against the allure of discounted surgical packages abroad, highlighting the importance of thorough research into the qualifications and accreditations of surgical facilities. These campaigns should articulate the potential for serious health consequences and the fact that the NHS may not cover all resulting treatment costs.
Ultimately, promoting greater regulatory oversight of overseas medical facilities and fostering collaboration with international healthcare organizations could assist in preventing similar incidents in the future.