Story Highlight
– GLP-1 drugs significantly reduce weight and heart attack risk.
– Reports of severe side effects, including pancreatitis, rising.
– Gallbladder removal surgeries increased by nearly 15%.
– Lawsuits filed over unreported severe side effects.
– Mental health effects still lack comprehensive research.
Full Story
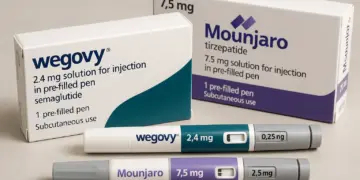
Recent evaluations of GLP-1 medications—namely, the weight-loss injections known as Wegovy and Mounjaro—have highlighted their significant benefits alongside concerning developments regarding their safety. While these drugs are often celebrated as groundbreaking in the battle against obesity, facilitating weight loss for millions and reducing the incidence of heart attacks and strokes by approximately 20% regardless of weight, a rise in reported side effects has raised questions about their long-term use.
Research published in BMC Medicine indicated that over 1.6 million adults across England, Wales, and Scotland sought treatment with these weight-loss injections between early 2024 and early 2025. As the popularity of GLP-1 medications surged, healthcare professionals have observed an alarming increase in hospital visits related to severe side effects, including persistent vomiting and dehydration. More worrisome, there has been a notable spike in conditions associated with gallbladder disease and acute pancreatitis, a critical inflammatory condition of the pancreas that can be life-threatening.
The Medicines and Healthcare products Regulatory Agency (MHRA) has recently adjusted its guidance for healthcare practitioners and patients due to a concerning uptick in incidents involving acute pancreatitis. The agency reported 1,143 cases linked to glucagon-like peptide-1 receptor agonists from 2007 to October 2025, which included 19 fatalities. Alarmingly, 973 of these reports and 17 deaths occurred within 2025 alone, highlighting the urgency of the situation.
The majority of these adverse events were associated with tirzepatide (brand name Mounjaro)—accounting for 807 reports—while 166 reports were linked to semaglutide (Ozempic and Wegovy). Additional reports included 146 instances related to liraglutide (Saxenda) and 61 involving dulaglutide. Current patient information leaflets for GLP-1 drugs, such as Mounjaro, indicate acute pancreatitis as an ‘uncommon side effect’, with occurrences affecting up to one in every 100 patients. However, the MHRA’s recent changes emphasise an elevated awareness of the “small risk of severe acute pancreatitis” in those prescribed these medications.
Parallel to the increase in acute pancreatitis cases, NHS England data revealed a near 15% rise in gallbladder removal surgeries in the past year, escalating from 69,745 in 2023-24 to 80,196 in 2024-25. Medical professionals attribute this surge to the growing use of GLP-1 medications. Notably, Professor Ahmed Ahmed, a gastrointestinal and bariatric consultant at Imperial College Healthcare Trust, highlighted the correlation, emphasising that these surgical fluctuations are uncommon year-on-year and strongly correlate with the recent spike in weight-loss injection use.
Gallstones, primarily formed from cholesterol, are recognised side effects of rapid weight loss, often induced by these drugs. Swift weight reduction prompts the liver to release additional cholesterol into bile, compounded by decreased gallbladder emptying, resulting in thicker bile and a higher likelihood of stone formation. Approximately 20% of individuals with gallstones may require gallbladder removal due to acute pain. This escalation in gallstone complications and subsequent surgeries correlates with an increase in reported acute pancreatitis cases, as gallstones can obstruct the pancreatic duct, triggering inflammation.
In recent developments, several patients in the United States have initiated legal action against the manufacturers of GLP-1 drugs, citing severe side effects, including vision problems, that were allegedly not disclosed. Legal firms in the UK reported similar enquiries from patients voicing concerns about potential harm from these medications.
The rising incidences of adverse effects echo patterns seen in the histories of past pharmaceuticals. For instance, Merck’s Vioxx, initially hailed for its favourable safety profile, was withdrawn from the market after emerging evidence linked it to cardiovascular risks following widespread use. Such phenomena highlight a systemic issue: long-term safety and effectiveness of medications often become more apparent only after extensive post-marketing observation.
Professor Sarah Jackson, of University College London, pointed out that clinical trials primarily focus on validating efficacy and identifying prevalent side effects, typically involving smaller patient populations in controlled settings. Consequently, unexpected complications may arise once a drug is widely accessible and administered to a broader demographic with diverse health backgrounds.
The use of GLP-1 drugs has escalated rapidly following their introduction for weight management in the UK in 2023, sparking concerns among medical professionals regarding the patient selection process and comprehensive risk understanding. While the MHRA frictionally updated its safety communications, indications suggest an urgency to reassess the current trajectory of GLP-1 prescription practices.
Integral to this discussion are the mental health implications potentially associated with GLP-1 medication use. Emerging research signals an increase in anxiety and depression rates among individuals utilizing these drugs. Meanwhile, some studies indicate that individuals with obesity and psychological conditions—often excluded from initial drug trials—may be at heightened risk for adverse mental health outcomes.
Insight and caution are necessary as the medical community confronts the implications of these medications on physical and psychological health. While proponents of GLP-1 treatments assert their substantial advantages in managing chronic conditions like diabetes and cardiovascular disease, they must be balanced with rigorous assessments of individual patient needs and potential risks. Ultimately, responsible prescribing guided by comprehensive patient evaluations will be imperative to harness the benefits of GLP-1 drugs while minimising harm.
Our Thoughts
To prevent the adverse effects associated with the increasing use of GLP-1 drugs, several key measures could be implemented. First, adherence to the Health and Safety at Work Act 1974 mandates that employers must ensure the health, safety, and welfare of employees, which encompasses proper prescribing practices and monitoring of patients on these medications.
Inadequate patient education and insufficient monitoring post-prescription highlight a failure to comply with the Misuse of Drugs Regulations 2001, which require proper oversight in the use of certain medications. Enhanced training for healthcare professionals about potential side effects, especially for new treatments like GLP-1s, could mitigate risks.
Additionally, clear and consistent patient information leaflets should emphasize all potential side effects, particularly concerning rare but serious conditions like pancreatitis and gallbladder disease, in alignment with the Consumer Protection Act 1987, which mandates the safety of products provided to consumers.
Furthermore, monitoring systems should be established to track and report adverse reactions comprehensively, ensuring rapid updates to clinical guidance. Improved patient screening and follow-up could also identify at-risk individuals before complications arise, adhering to the principles of the Health and Social Care Act 2008, which stipulates that care must be safe and responsive to patients’ needs.