Story Highlight
– Ultra-processed foods comprise nearly half of daily calories.
– Children are among the highest consumers of UPFs.
– Industry influence delays effective regulation and public health action.
– Regulatory frameworks for UPFs are fragmented and outdated.
– Authors recommend stricter regulations and healthier food subsidies.
Full Story
In recent years, ultra-processed foods (UPFs) have emerged as a significant contributor to daily calorie consumption in numerous countries, particularly among children. Despite mounting evidence linking these foods to adverse long-term health outcomes, regulatory measures have not kept pace with the growing concerns.
A detailed examination of this issue is presented by Professor John O Warner from Imperial College London and Alisha Khan, a medical student from The University of Sheffield, in a recent article for Future Healthcare Journal (FHJ). The authors argue that the leniency in regulation surrounding UPFs is largely due to the disproportionate influence exerted by the manufacturers of these products, compounded by outdated and fragmented policy frameworks. They contend that this situation persists despite substantial scientific evidence highlighting the potential dangers associated with UPF consumption.
Defining UPFs, Warner and Khan explain that these foods are typically characterised by a long list of ingredients that would not normally be present in home-cooked meals. They are often laden with artificial additives including azo dyes—predominantly used to enhance colour—non-caloric sweeteners, emulsifiers, and various preservatives. The concern is that these additives not only disrupt the gut microbiome but also impair the body’s natural mechanisms that protect against chronic diseases. Moreover, some additives, such as azo food dyes, may even be metabolised into compounds that damage DNA, raising alarms over potential carcinogenic effects.
The authors further illustrate how UPFs can lead to “hedonistic hunger,” a phenomenon where individuals consume food even when not driven by physical hunger. This tendency can result in overeating and contribute to the global obesity crisis. Their appealing appearance, affordability, and convenience make these foods especially popular, albeit at the expense of nutritional value. Notably, recent research has suggested parallels between the effects of UPFs and tobacco use, indicating both are engineered to foster addiction and overconsumption.
In addressing the lack of robust regulation, Warner and Khan delineate three primary factors that impede effective policy change: the influence of the food industry on government regulations, the outdated regulatory frameworks that govern food safety, and the erratic public health strategies as a result of competing political and commercial interests.
The authors assert that vested interests within the food and advertising sectors significantly obstruct public health initiatives aimed at tackling UPFs. There have been cases where industry lobbying has successfully thwarted local attempts to impose advertising restrictions—often by threatening a loss of income linked to advertising revenue. Historical examples, such as research funded by the sugar industry that sought to downplay links to heart disease, demonstrate how corporations can manipulate scientific dialogue to protect their interests. Warner and Khan express concern that similar tactics could be at play in the realm of UPFs, wherein companies engage in ‘healthwashing’ to mislead consumers about the safety of their products, such as highly processed alternatives marketed as healthier options.
In terms of regulatory frameworks, the authors highlight a significant degree of inconsistency and fragmentation. For instance, while some European nations have removed approval for certain harmful food colourants due to health concerns, regulatory bodies like the Food and Drug Administration (FDA) and the European Food Safety Authority continue to endorse their use. This dissonance creates confusion about the safety of various additives and distracts from the urgent need to develop comprehensive nutrition policies that address the overarching risks associated with UPFs.
Moreover, public health strategies concerning UPFs are frequently riddled with inconsistencies, often undermined by external commercial pressures. The trend of manufacturers moving from sugar to non-caloric sweeteners is noted, despite a lack of evidence supporting that non-caloric sweeteners are a healthier alternative. In some Californian cities, for example, taxes have been implemented on sugary drinks, yet it remains unclear if beverages containing non-caloric sweeteners will fall under similar regulations.
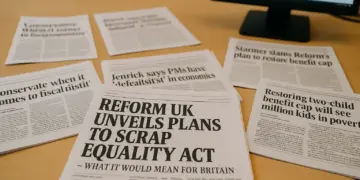
In the UK, similar dynamics are at play. The authors describe how political pressures have compelled changes in government guidance for food outlets, influenced by entities like the Food and Drink Federation, which represents major multinational corporations. This has led to legislation that addresses only those products high in fat, sugar, or salt, while completely omitting any reference to processed or ultra-processed foods.
In light of these challenges, Warner and Khan propose several critical reforms. They advocate for the introduction of clearer, more stringent regulations governing UPFs, including the replacement of the antiquated E number system with labels that clearly identify safe additives. Additionally, they suggest implementing prominent front-of-pack warnings on products containing harmful ingredients, outright bans on high-risk additives such as azo dyes, and stricter marketing regulations, especially those targeting children.
To ensure fresh foods become more viable alternatives, the authors recommend subsidy initiatives aimed at reducing prices. Furthermore, they call for the establishment of an independent national taskforce that can objectively assess evidence, minimise industry influence, and direct coherent policy reforms focused squarely on public health outcomes.
Through these recommendations, the authors hope to stimulate action that prioritises the health of vulnerable populations and confronts the pervasive issue of UPFs in contemporary diets. The growing body of research underscores the urgency of addressing this public health concern, from advocating for clearer regulations to fostering a healthier food environment for all.
Our Thoughts
The article highlights significant failures in the regulation of ultra-processed foods (UPFs) in the UK, which contribute to long-term health risks, especially for vulnerable populations. Key lessons include the need for more robust regulatory frameworks that limit industry influence and prioritize public health. Current health legislation, including the Food Safety Act 1990 and the Health and Safety at Work Act 1974, shows gaps in addressing the health impacts of food additives and UPFs comprehensively.
To prevent similar incidents, regulatory actions could include updating food safety regulations to restrict harmful additives like azo dyes, enhancing labeling requirements for consumer transparency, and imposing stricter marketing limits aimed at children. The lack of cohesive public health strategies must be addressed to unify approaches against UPFs, avoiding fragmented policies that fail to protect consumers effectively.
The influence of food industry lobbyists on public health regulations undermines the precautionary principle, a core component of UK health and safety legislation. Hence, establishing an independent body to evaluate health evidence and mitigate industry pressures could be vital in reforming food regulations and safeguarding public health.