Story Highlight
– Women received over £600,000 in damages for surgery mistakes.
– Surgeon Derek Klazinga left patients in chronic pain.
– Vaginal mesh use halted in UK due to safety concerns.
– Betsi Cadwaladr Health Board acknowledged consent failures.
– Klazinga retired before facing medical practice evaluation.
Full Story
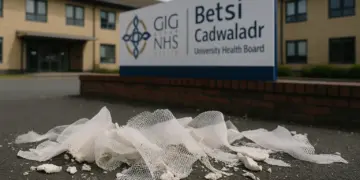
A group of women affected by inadequate gynaecological procedures performed by a former NHS surgeon has successfully sought compensation exceeding £600,000. The incidents tied to these medical failures occurred under the care of Derek Klazinga, who operated as a consultant for the Betsi Cadwaladr University Health Board in North Wales from 2002 until 2016.
Mr Klazinga was involved in numerous surgeries involving the implantation of a device known as vaginal mesh. This surgical product, designed to support pelvic organs in cases of incontinence or pelvic organ prolapse, was subject to increasing safety scrutiny, leading to a suspension of its use in the UK in 2018. Reports suggest that many women have since endured extended periods of discomfort and medical complications due to these procedures.
As of an investigative report aired by the Welsh-language broadcaster S4C, it has been revealed that at least 25 women have received compensation related to their treatment by Mr Klazinga. Notably, seven of them received a combined total of £600,000 since 2015. Kerry Watson, a 40-year-old from Kinmel Bay in Conwy, is among those affected. After undergoing surgery for bladder prolapse when she was 29, Watson has since faced ongoing medical challenges, requiring as many as 120 tablets weekly to manage her pain. In 2024, she was also diagnosed with post-traumatic stress disorder (PTSD).
Reflecting on her ordeal, Watson shared her harrowing experience, stating, “I didn’t want to be here anymore. I couldn’t deal with the pain, I couldn’t deal with the thoughts I had. I was nobody, just a bag of pain. Ten long years of that. Ten long years.” Following the surgery, she described waking up in unbearable discomfort, specifically noting, “When I woke up the next morning, I had this awful pain in my back, on the left side. The pain was off the scale. I’ve never felt anything like it.”
Watson recounted difficulties she faced in daily life because of her condition, including challenges while caring for her three children. “I was leaking when I exerted myself or tried to play with the boys or pick them up,” she explained, underscoring how her health issues extended beyond mere physical pain.
In 2023, after coming across a law firm’s website focusing on legal cases related to the Betsi Cadwaladr health board, Watson pursued her own legal action. Medical reviews indicated that she had not needed surgical intervention in the first place; a consultant suggested that less invasive treatments such as injections or a removable device known as a pessary could have sufficed to manage her symptoms more effectively. While the health board contested the viability of injections as an option, they accepted that alternative non-surgical routes, such as pessary devices, should have been discussed with Watson prior to her surgery. Furthermore, they acknowledged that the process of securing her informed consent had fallen below acceptable standards.
“I wasn’t told about the risks involved with mesh. I didn’t receive the correct information before the surgery,” Watson stated, underlining her disappointment with the healthcare she received. Her payout was predicated on the argument that she was not presented with an alternative procedure to the tension-free vaginal tape obdurator (TVT-O) surgery she underwent, and that she was inadequately informed about the risks associated with the operation.
Watson noted, “I was initially offered a low amount, so I declined their first offer. I ended up accepting £110,000 and then fees are taken off that.” After covering legal expenses, her net compensation amounted to £97,200, a sum she expressed as inadequate given the emotional and physical toll her experiences have taken: “Is that going to cover all those nights I’ll be up crying in pain? That doesn’t touch the sides, really.”
Several women have come forward to relay similar accounts, and a number have stated they lacked full consent for their procedures. Chronic pain and its significant impact on daily life have been common themes in the testimonies shared, particularly on the S4C TV programme Y Byd ar Bedwar.
The Betsi Cadwaladr University Health Board did not disclose the total amount paid out to the 25 patients implicated in these claims, citing data protection issues. However, they did confirm that over £5 million in compensation has been distributed over the past decade due to medical errors in gynaecological procedures.
Michael Strain, a solicitor representing one of the claimants, described the situation as a significant scandal, calling for enhanced transparency regarding patient safety and medical accountability. He remarked on the abnormality of one clinician being associated with a large number of claims, particularly in instances where the healthcare board did not communicate this information to affected patients.
Derek Klazinga opted to remove himself from the medical register in 2021, prior to a scheduled fitness-to-practise hearing with the General Medical Council, which consequently did not occur. In a statement, he expressed his sympathy for the suffering endured by the women involved, attributing the issues to “defective medical products” that were eventually identified as harmful and banned in 2018.
Mr Klazinga asserted, “I ceased practising medicine ten years ago, more than two years before the ban,” emphasising his commitment to patient care and integrity during his practice. However, the specific manufacturer of the mesh used in these cases remains unidentified, though some companies have issued compensation for complications without admitting responsibility.
Dr Clara Day, the Executive Medical Director of BCUHB, issued an apology for the distress caused to women who’ve experienced complications following mesh insertions. She acknowledged historical claims linked to Mr Klazinga and highlighted the board’s compliance with legal processes in addressing these complaints. Dr Day asserted that the health board has taken steps to learn from these cases, promoting continuous improvement within the organisation.
The overarching implications of these cases highlight the need for ongoing scrutiny of medical practices in the UK, particularly concerning the consent process and patient safety standards. The full investigative report is available on the S4C programme Y Byd ar Bedwar on BBC iPlayer, complete with English subtitles.
Our Thoughts
The incidents involving flawed gynaecological surgeries by NHS surgeon Derek Klazinga highlight significant breaches of UK health and safety regulations, particularly those related to informed consent under the Care Quality Commission (CQC) standards and the Health and Social Care Act 2008. The health board admitted that alternative treatment options were not appropriately discussed with patients, violating patient rights to informed decision-making.
To avoid such outcomes, thorough risk assessments and comprehensive consent processes, as stipulated by the General Medical Council’s guidelines on consent, should have been diligently implemented. Enhanced training and oversight for clinicians, particularly for complex procedures involving potentially harmful products like vaginal mesh, are crucial. Regular audits and surveillance of medical outcomes would enable the identification of patterns of malpractice, promoting a culture of accountability and patient safety.
Lessons learned include the importance of transparent communication in medical settings and rigorous adherence to established protocols to safeguard patient welfare. Future incidents can be mitigated by mandating multi-disciplinary reviews for invasive surgeries and actively engaging patients in discussions about alternative treatments, ensuring they are fully informed of all risks and benefits prior to consent.