Story Highlight
– Nine-year-old Dylan Cope died from sepsis after discharge.
– Hospital misdiagnosed appendicitis as influenza, ignoring GP’s notes.
– Coroner ruled death resulted from “gross failure of care.”
– Mother campaigns for awareness to prevent similar tragedies.
– New safety-netting leaflets aim to improve patient care.
Full Story
A nine-year-old boy from Newport tragically lost his life to sepsis after being wrongly discharged from hospital with a flu diagnosis, despite a general practitioner’s (GP) warning of potential appendicitis. An inquest has since established that if appropriate surgical intervention had occurred for a burst appendix, Dylan Cope’s death could have been prevented.
Dylan, who passed away on December 14, 2022, had been taken to the emergency department at Grange University Hospital in Cwmbran with severe abdominal pain. Initially, Dr. Amy Burton, his GP, suspected appendicitis and promptly referred him to the hospital, alerting the healthcare team of her concerns.
At the hospital, Dylan was attended by paediatric nurse practitioner Samantha Hayden. However, key information from Dr. Burton regarding the suspicion of appendicitis was overlooked in the course of Dylan’s examination. Hayden later described the day as “exceptionally busy,” indicating that the high demand on services may have contributed to the oversight.
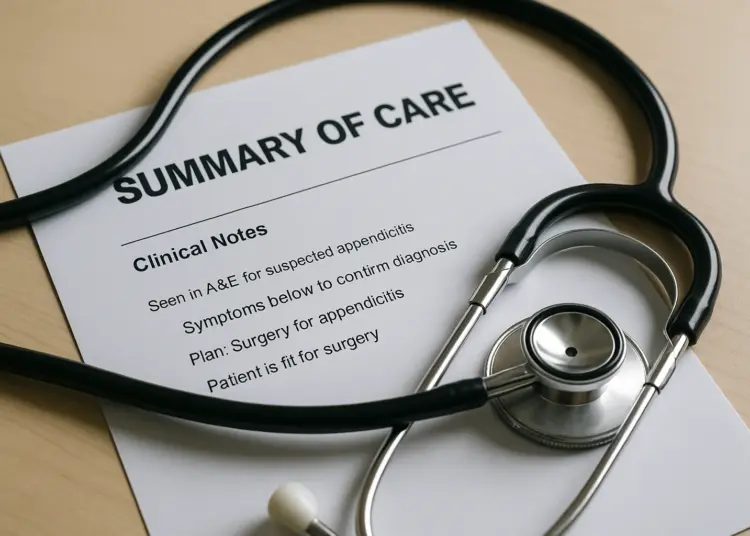
Dylan was subsequently examined by an unspecified clinician, who overlooked the concerns regarding his appendix, leading to his discharge with ibuprofen and a leaflet for treating colds in children. Unfortunately, this decision meant that urgent care for a potentially life-threatening condition was missed.
In the following days, Dylan’s health deteriorated. His family experienced a frustrating wait for a callback from NHS services, during which time Dylan displayed severe symptoms indicative of sepsis, including the mottling of his legs, a condition that can signal critical illness. In light of his worsening state, Dylan’s father made a swift return to the A&E department, where his condition was assessed, and it became evident that his appendix had indeed ruptured.
Amid a harrowing development, medical staff at the University Hospital of Wales ultimately communicated the grim prognosis: Dylan’s chances of survival were alarmingly slim. Efforts to keep him alive were made, but life support was gradually withdrawn, and he succumbed to sepsis, with the coroner’s inquiry later revealing that neglect played a significant role in his untimely death.
Corinne, Dylan’s mother, has since advocated for greater awareness and preventative measures against such tragic occurrences. She poignantly expressed the residual “lifetime of pain” that follows the loss of a child, emphasising that despite her efforts to push for change, the grief remains profound. As she stated, “The death of a child, particularly when you know that it’s preventable, is just really complex… It’s a life sentence of pain.”
In the wake of Dylan’s death, Corinne began a campaign aimed at addressing systemic failures in the healthcare process, particularly focusing on improving communication and safety protocols within hospitals. She discovered that certain resources, like the “Spotting the Unwell Child” leaflet, which is prevalent in England, were not available in Wales. In collaboration with the UK Sepsis Trust, she has been working to promote these resources in hopes of preventing similar tragedies in the future.
Her advocacy has already led to the development of All-Wales safety-netting leaflets intended for both adults and children. These leaflets are designed to educate parents and caregivers about warning signs of serious conditions like sepsis and include QR codes linking to relevant NHS resources. “Safety-netting is important because parents can’t be relied on to remember every detail, particularly when they are tired and worried,” Corinne explained, reinforcing the idea that robust information must be readily accessible.
The Welsh Government has acknowledged the need for improved resources, agreeing to incorporate the UK Sepsis Trust screening tools into public health initiatives. This development aims to equip patients with the knowledge to assess symptoms while awaiting medical assistance, ensuring that early intervention can occur when necessary.
As Corinne continues her campaign, she is resolute in her belief that timely recognition of symptoms and optimal care can save many lives, stating, “Not every death is preventable, but a lot of them are with timely recognition and optimal care.”
The Aneurin Bevan University Health Board, responsible for the care that Dylan received, has accepted the coroner’s findings and acknowledged its responsibility for the failings highlighted in his case. This admission underscores the ongoing need for improvements within the health system, as such tragedies reveal significant gaps that can lead to devastating outcomes for families.
Dylan’s story stands as a stark reminder of the importance of thorough medical assessments and the critical nature of communication between healthcare providers. As Corinne looks to the future, she hopes her efforts will contribute to a healthcare system where preventable deaths become increasingly rare, fostering safer environments for children and families.
As she reflected on her journey, Corinne poignantly remarked, “Dylan and many others like him—their lives and preventable deaths—are not in vain. It can’t all be for nothing.” Her resilience and determination highlight the ongoing struggle for change in healthcare practices, ensuring that such heart-wrenching losses do not occur in vain.
Our Thoughts
The tragic case of Dylan Cope highlights significant failings in patient assessment and care, ultimately leading to his preventable death from sepsis. Key safety lessons include the necessity of thorough communication between medical professionals and adhering to established protocols for handling suspected appendicitis. The hospital’s disregard of the GP’s notes and the paediatric nurse practitioner’s failure to follow up on the initial diagnosis constitute breaches of the Care Quality Commission’s regulations regarding safe and effective care.
To prevent similar incidents, hospitals must implement robust safety-netting procedures and ensure that all medical personnel receive proper training on the interpretation and prioritization of referrals and notes from GPs. The introduction of standardized patient discharge procedures, particularly for cases involving possible surgical interventions, would be beneficial. Furthermore, adopting and utilizing safety-netting leaflets as proposed by Dylan’s mother can help empower families by providing clear guidance on recognizing deteriorating health conditions.
Overall, a systemic review of protocols and stricter adherence to patient safety guidelines in line with UK Health and Safety legislation, including the Health and Safety at Work Act 1974, could significantly reduce the risk of such tragedies in the future.