Story Highlight
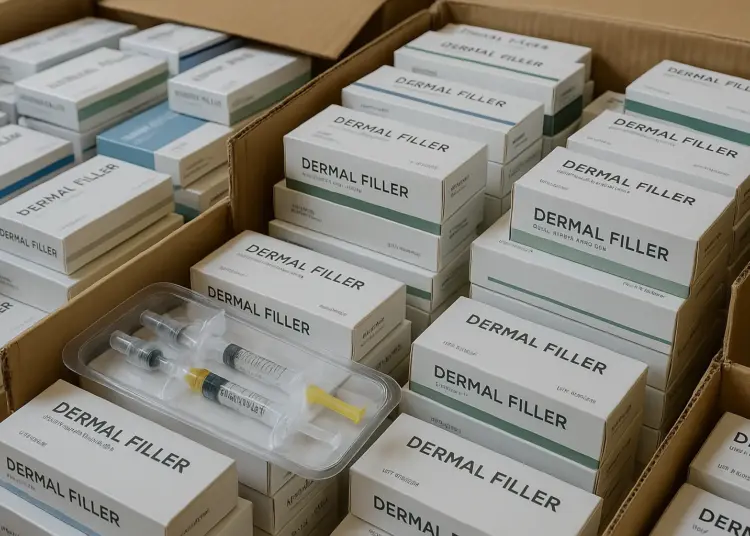
– £4m worth of illegal fillers seized by MHRA.
– Over 27,000 unlicensed dermal fillers confiscated since 2020.
– Counterfeit fillers pose risks of disfigurement and infection.
– Experts warn against low-priced fillers and unlicensed providers.
– MHRA reports significant illegal medicine seizure in 2025.
Full Story
Counterfeit dermal fillers valued at up to £4 million have been confiscated by UK regulators, following alarming warnings from dermatologists about the potential health risks associated with these unlicensed products. Since January 2020, the Medicines and Healthcare products Regulatory Agency (MHRA) has seized more than 27,000 units of these fillers, with the majority of confiscations occurring in 2023 when 19,754 units were removed from circulation.
The MHRA has underscored the dangers posed by these illicit fillers, stating that they can “put your health at risk” as these products lack any regulatory oversight. There are no guarantees regarding their quality or safety, and the ramifications of using such products can be severe.
A recent freedom of information (FOI) request by Vip Italia, a cosmetics company, revealed stark statistics about the prevalence of counterfeit fillers, highlighting a staggering increase in seizures this year compared to previous years, which saw only 631 units taken in 2022. The financial implications of these findings are significant; although the MHRA does not disclose exact valuations, industry estimates suggest that the seized products could be worth between £677,450 and potentially as much as £4 million, as retail prices for dermal fillers can range from £25 to £150 per unit.
Dermal fillers are primarily used for cosmetic enhancements, including the reduction of wrinkles and skin revitalisation. However, their misuse carries considerable health risks. “The filler should be clear and smooth, never cloudy or clumpy,” advises Dr Raoul Novelli, a plastic surgeon based in Milan. He warns that if the syringe is not robust or lacks a clearly printed brand name, it is likely a counterfeit product.
Dr Emma Wedgeworth, a consultant dermatologist and representative for the British Skin Foundation, expressed deep concern about the dangers presented by counterfeit fillers. “Counterfeit fillers are potentially incredibly dangerous. They are not subject to regulations essential to prevent devastating complications. Using these can put people at risk of disfigurement and infection, which can cause huge health issues,” she explained.
Experts highlight that the risks associated with counterfeit fillers are not limited to the composition of the product itself. Dr Novelli elaborated on the dangers of improper administration. Injecting fillers too close to blood vessels can result in serious complications, including blocked arteries, tissue necrosis, infections, scarring, and nerve damage. Other aesthetic issues may include asymmetry, overfilling, and skin discolouration.
Nora Nugent, consultant plastic surgeon and president of the British Association of Aesthetic Plastic Surgeons (BAAPS), raised important points about identifying red flags when choosing a clinic. “One of the biggest warning signs that a clinic may be selling counterfeit fillers is if their prices are significantly lower than competitors. Always be cautious when fillers are offered at very low prices,” she advised. “Unlicensed fillers typically are cheaper or are provided outside of a medical setting by unqualified practitioners. These practices pose safety risks, and the potential dangers greatly outweigh any superficial benefits you might gain.”
Further advice from Vip Italia suggests that consumers should be vigilant when it comes to verifying the legitimacy of fillers. Fake vials often lack batch numbers or expiration dates, which are crucial for ensuring the product’s safety and efficacy. “The filler should be clear and smooth, never cloudy or clumpy. If the syringe looks flimsy or doesn’t have the brand name printed clearly on it, it’s likely a fake,” reiterated Dr Novelli.
This new data comes against a backdrop of wider concerns regarding the illegal trade of medicines in the UK. Earlier reports indicate that the MHRA seized nearly 20 million doses of illicitly traded medications in 2022, with an estimated street value approaching £45 million. An MHRA spokesperson noted the importance of purchasing medicines from regulated suppliers, warning that “buying any medicine from illegally trading online suppliers significantly increases your risk of receiving a product which is not licensed for use in the UK. Purchasing from illegal suppliers means there are no safeguards to ensure that it meets our quality and safety standards. Taking such medicines may put your health at risk.”
As the popularity of cosmetic procedures continues to rise, the dangers presented by counterfeit products remind consumers to exercise caution. Awareness and education around the risks associated with counterfeit fillers and medications are crucial to safeguarding public health. The vigilance of health authorities, coupled with informed choices by consumers, is vital in combating the threat posed by counterfeit medical products.
Our Thoughts
The recent seizure of illegal dermal fillers highlights significant gaps in regulatory enforcement and consumer safety in the UK. To prevent such incidents, stricter regulations should be enforced regarding the sale and distribution of cosmetic products. Key lessons include the need for enhanced public awareness on the risks associated with unlicensed fillers and the importance of purchasing such products from reputable medical professionals only.
Relevant regulations that may have been breached include the Medicines Act 1968 and the Health and Safety at Work Act 1974, which mandate the safe handling and distribution of medical products. Failure to comply with these regulations poses risks of disfigurement and infection, as highlighted by dermatologists.
To avoid similar incidents in the future, it is crucial to implement robust monitoring and enforcement mechanisms by the MHRA, including stricter penalties for illegal suppliers. Additionally, healthcare practitioners should be required to verify the authenticity of products used in treatments, ensuring they possess clear labelling, batch numbers, and expiry dates. Public education campaigns could also be beneficial in informing consumers about identifying counterfeit risks and the importance of seeking treatments in licensed medical environments.