Story Highlight
– MHRA warns GLP-1 drug users of serious side effect.
– Look for severe stomach and back pain symptoms.
– 1.6 million people in UK used GLP-1s recently.
– Ozempic, Wegovy, and Mounjaro linked to pancreatitis risk.
– Seek medical help if severe pain occurs.
Full Story
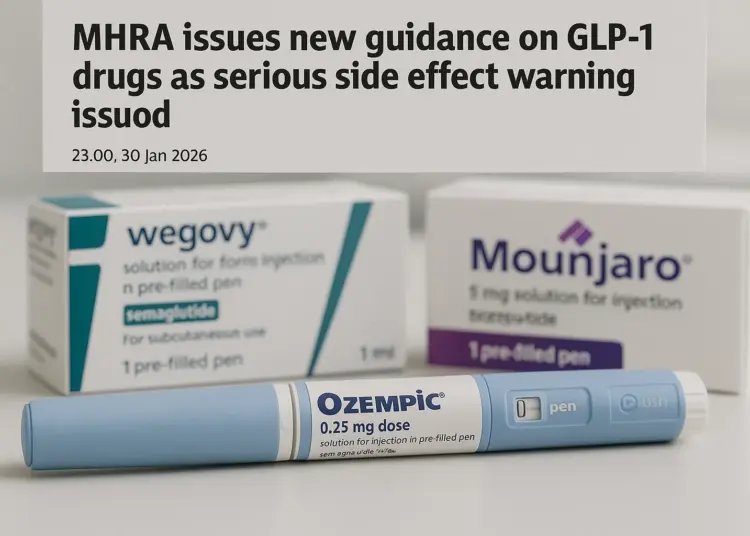
Patients and healthcare professionals are being alerted to a rare but serious potential side effect linked to GLP-1 (glucagon-like peptide-1) medications, according to new guidance from the Medicines and Healthcare products Regulatory Agency (MHRA). These drugs, which include widely used options such as Ozempic, Wegovy, and Mounjaro, have gained popularity in the UK, with approximately 1.6 million individuals reportedly receiving these injections over the past year for weight management.
The MHRA’s latest update highlights the importance of being vigilant for symptoms that may indicate acute pancreatitis, a condition characterised by inflammation of the pancreas, which is situated behind the stomach. The agency has urged anyone using GLP-1 medications to seek immediate medical attention if they experience severe, persistent abdominal pain, particularly if this pain extends to the back, as well as accompanying symptoms like nausea and vomiting.
While most patients who develop acute pancreatitis can recover within a week and typically do not face ongoing issues, the NHS warns that some may experience more serious complications. In light of this, the MHRA has amended product information for healthcare professionals and patients to ensure awareness of the risks associated with these medications.
Alison Cave, Chief Safety Officer at the MHRA, emphasised the agency’s commitment to patient safety: “Patient safety is the MHRA’s top priority and we continually monitor the safety and efficacy of all licensed medicines.” She reassured patients that the majority of people taking GLP-1 medications do so without significant issues, noting, “For the vast majority of patients who are prescribed GLP-1s, they are safe and effective medicines which deliver significant health benefits.”
The MHRA’s guidance serves as a critical reminder for both patients and physicians to remain alert to possible symptoms of acute pancreatitis. Cave further advised that if anyone using GLP-1 medications observes symptoms such as intense stomach pain or signs of nausea and vomiting, they should consult a healthcare professional promptly and report the occurrence through the MHRA’s Yellow Card scheme, which is designed for monitoring drug safety.
Various brands of GLP-1 medications have differing indications. While Wegovy and Mounjaro are specifically licensed for weight management, Ozempic is approved for the treatment of type 2 diabetes and for reducing cardiovascular risk. According to the MHRA, these medications are used not only for diabetes management but also to assist individuals with a BMI of 27 kg/m² or more in reducing weight and cardiovascular risk if they have existing cardiovascular disease.
A study conducted by University College London has disclosed the extensive use of GLP-1 medications across England, Wales, and Scotland, asserting that around 1.6 million adults have utilised them over a year-long period to facilitate weight loss. It underscores the growing trend and acceptance of these treatments, which have emerged as critical tools in the management of both obesity and type 2 diabetes.
However, the necessity for ongoing vigilance regarding potential risks associated with any medication cannot be overstated. Although GLP-1s are widely regarded as safe and effective for their intended purposes, like any therapeutic intervention, they come with certain risks which require acknowledgment from patients and prescribers alike. The MHRA has made it clear that understanding the symptoms of severe pancreatitis is crucial for those utilising GLP-1 treatments.
Patients experiencing acute pancreatitis often report a sudden onset of severe pain in the centre of the abdomen, which can be accompanied by nausea or vomiting. A high temperature of 38 degrees Celsius or more could also indicate the condition. In cases where any of these symptoms develop unexpectedly, individuals are encouraged to seek immediate medical advice, whether through a general practitioner or NHS 111, ensuring timely intervention can take place.
The MHRA’s updated guidance reflects an ongoing commitment to ensuring that the benefits of medications like GLP-1s do not come at the expense of patient safety. In recent years, there has been increasing scrutiny of pharmaceutical products as they become integral to treating chronic conditions like obesity and diabetes. With the rise of these medications, informed decision-making by patients and healthcare providers is more essential than ever.
Maintaining awareness of potential side effects enables patients to take an active role in their health management, reinforcing that while GLP-1 drugs provide significant health improvements, awareness and prompt action regarding adverse symptoms is vital. The MHRA continues to urge both prescribers and patients to remain informed and proactive in addressing any concerns that may arise during treatment.
Our Thoughts
To mitigate the risks associated with GLP-1 drugs and prevent incidents of acute pancreatitis, several measures could have been taken. Firstly, enhanced pre-prescription risk assessments based on the patient’s medical history could ensure only suitable candidates receive these medications. This would align with the Health and Safety at Work Act 1974, which mandates ensuring the health and safety of individuals using medicines.
Secondly, there should be a structured monitoring system post-prescription for early detection of adverse effects, facilitating prompt intervention. Clear and consistent communication of potential side effects, beyond product information, could empower patients to recognize symptoms early, adhering to the Control of Substances Hazardous to Health Regulations (COSHH).
Key safety lessons include the importance of continuous education for healthcare professionals regarding emerging risks, ensuring compliance with the Medicines Act 1968, which governs the safety of medicines. The MHRA’s guidance highlights the need for vigilant monitoring and reporting of side effects through methods like the Yellow Card scheme. Overall, proactive measures in patient education and healthcare professional training are essential to prevent similar incidents effectively.