Story Highlight
– Over 295,000 violent incidents reported by NHS staff, 2022-2025.
– Surge in assaults during Christmas and New Year seasons.
– Nearly 24,000 sexual assault cases reported over three years.
– Staff face increasing danger from patients with mental health issues.
– Calls for urgent action to ensure staff safety and protection.
Full Story
NHS staff, including nurses, doctors, and paramedics, are facing alarming levels of violence and abuse, with reports indicating tens of thousands of incidents each year. This troubling trend has been characterised as a national crisis for healthcare workers in the UK. Recent data obtained through freedom of information requests highlighted that between 2022 and 2025, over 295,000 incidents of violence and aggression against NHS staff were recorded across 212 trusts in England.
Healthcare unions have expressed deep concern about a disturbing increase in assaults, notably during the Christmas and New Year periods. A recent incident in Merseyside involved a man attacking staff and patients at Newton Community Hospital with a crowbar, resulting in multiple injuries. This individual was subsequently arrested and detained under the Mental Health Act by local authorities.
Data analysis indicates a significant uptick in violent incidents, with reported cases rising from 91,175 in the 2022-2023 period to 104,079 by 2024-2025. This equates to roughly 285 incidents reported daily in the latest year alone. The Royal College of Nursing (RCN) General Secretary, Professor Nicola Ranger, has emphasised the severity and frequency of these assaults, labelling the situation a “national emergency” concerning staff safety.
There has also been a noted increase in instances of sexual violence and harassment directed at NHS staff, with nearly 24,000 incidents reported over the last three years—an increase from around 20,000 in the preceding five years. Some healthcare workers have relayed personal experiences of sexual assault while attending to patients, and there have been alarming reports of patients engaging in deliberate acts of sexual harassment.
“Working in the NHS is becoming increasingly dangerous,” Professor Ranger remarked. She further articulated the outrage that should accompany the reality faced by healthcare professionals, particularly in nursing, which is dominated by female staff who are often vulnerable to both physical and sexual assault.
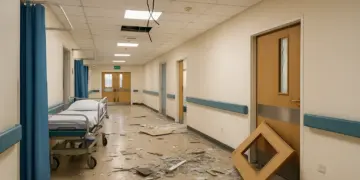
Healthcare professionals have outlined a wide spectrum of violent behaviour, including assaults involving weapons, destruction of hospital property, and resulting financial losses running into hundreds of thousands of pounds. Alarmingly, the individuals responsible for these assaults often evade repercussions, such as treatment bans or legal prosecution.
According to the British Medical Association (BMA), the escalation in violence from patients can be attributed to a mix of factors such as frustration due to prolonged wait times, a growing mistrust in medical practices heightened by Covid-19 conspiracy theories, and an alarming rise in racially motivated incidents involving staff of colour. Emma Runswick, deputy chair of the BMA council, stated that NHS employees are increasingly living in fear of harassment and violence.
Frontline staff have described a worrying trend where entire hospital wards are frequently shut down to isolate violent young patients, particularly those with severe mental health conditions or autism, due to a lack of appropriate specialist care. One risk manager from a major NHS trust revealed that wards could be locked down for months, leading to a situation where members of security overshadow healthcare staff. Such environments can be dangerous, with past incidents resulting in severe damage to hospital property.
Runswick recounted numerous episodes where patients with acute mental health issues have necessitated heightened security and staffing measures. In her experience, some teenage patients required around-the-clock supervision from multiple staff members to prevent them from inflicting harm on themselves or others. She pointed out that frustration and violence often stem from the inadequate nature of services and long wait times.
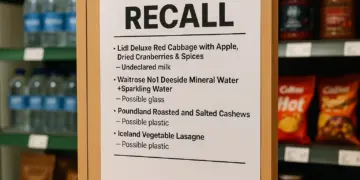
Amid these challenges, healthcare unions have raised serious questions about the accuracy of assault data, suggesting that actual numbers may be significantly higher than reported. Of the trusts surveyed, 40 recorded over 2,000 alleged violent incidents each during the 2022-2025 period, with several surpassing 5,000. In contrast, a handful of trusts reported disturbingly low figures, which experts have deemed implausible given the substantial number of staff and patients involved.
The RCN noted that many healthcare professionals may not formally report incidents due to the frequent nature of assaults, exacerbating the issue of underreporting. “These figures show that some trusts are dealing with explosions in incidents, while others refuse to share data or claim they’ve barely had a single case,” added Professor Ranger.
A recent RCN survey involving 20,000 nurses indicated that over 27% experienced physical assaults while working, while more than 10% reported incidents of sexual harassment. Professor Ranger urged Health Secretary Wes Streeting and NHS England to take decisive action to address the escalating crisis, highlighting that some trusts are likely failing to meet their legal responsibilities under health and safety legislation.
Runswick concurred, suggesting that many trusts requiring inspection under the Health and Safety Executive could be found negligent in their responsibilities to prevent violence and harassment. She noted a disheartening trend where NHS trusts often profess a zero-tolerance policy but fail to implement effective measures to protect their staff.
In response to these critical findings, Health and Social Care Secretary Wes Streeting acknowledged that violence and aggression towards NHS personnel are wholly unacceptable. “Our doctors, nurses, and healthcare workers deserve to feel safe at work without fear of abuse, assault or harassment,” he stated. Furthermore, he outlined initiatives for trusts to bolster staff training and swiftly address incidents of misconduct.
An NHS England representative echoed this sentiment, describing physical violence against staff as “totally unacceptable” and encouraging victims to report such incidents to authorities. Additionally, a spokesperson from the National Police Chiefs’ Council affirmed their commitment to a zero-tolerance policy against any form of violence, ensuring that those serving on the frontline can carry out their essential duties without fear.
Our Thoughts
To mitigate the rising incidents of violence and sexual assaults against NHS staff, several key measures could have been implemented. Firstly, a thorough risk assessment in line with the Health and Safety at Work Act 1974 should be conducted to identify potential hazards and implement effective control measures. Enhanced training programs focused on de-escalation techniques could better prepare staff for handling aggressive patients.
Institutions should ensure compliance with the Management of Health and Safety at Work Regulations 1999, which mandates employers to conduct regular evaluations of safety procedures and provide adequate support for staff. Establishing a robust reporting mechanism is essential to ensure all incidents are documented accurately, as underreported incidents hinder the effectiveness of safety strategies.
Given the alarming reported increase in assaults and harassment, NHS trusts may be in breach of the Equalities Act 2010 regarding the protection against discrimination and harassment in the workplace.
Strengthening collaboration with security services, improving psychiatric care, and ensuring a zero-tolerance policy towards abusive behavior could also foster a safer environment. Consistent enforcement of penalties against perpetrators can deter future incidents, creating a culture of accountability within the healthcare setting.