Story Highlight
– Emma faced uncertainty about medication safety during pregnancy.
– Over 90% of medicines untested in pregnancy situations.
– WHO aims to improve drug safety testing for pregnant women.
– Historical neglect of pregnant women in clinical trials noted.
– Need for autonomy and informed choices for pregnant patients.
Full Story
Emma, a 35-year-old woman living with Ehlers-Danlos syndrome, found herself facing a difficult decision when she and her partner chose to start a family. The challenges of her condition, which severely affects her connective tissues, include the loss of her bladder and reliance on a feeding tube for nutrition. As she began discontinuing some of the medications that supported her daily life, she encountered a significant uncertainty: the potential effects of her remaining medications on her unborn child. “The vast majority of the information that’s available is like, ‘to be used if there’s no other options, no research done’. And without the medication I will end up in hospital so I don’t really have an option but to take it,” said Emma. This lack of clarity surrounding the safety of these medications has led to feelings of both guilt and anxiety.
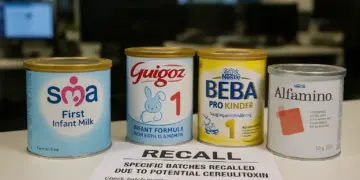
The reality Emma faces is not unique; it reflects a broader issue affecting pregnant women around the globe. Alarmingly, over 90% of medications have not undergone testing in pregnant populations. This gap leaves many women grappling with the dilemma of whether to forgo necessary treatments or proceed without the reassurances typically offered in clinical practice. In a significant move to address this critical issue, the World Health Organization (WHO) has announced a collaboration aimed at rolling out an initiative that could transform the landscape of drug testing in relation to pregnancy.
This initiative comes in the wake of cautionary tales from the past, particularly the Thalidomide tragedy of the 1950s and 1960s. Thalidomide was prescribed to pregnant women for morning sickness before it became evident that the drug was responsible for serious birth defects, such as limb malformations. This tragic event catalysed reforms that established stringent safety monitoring for pharmaceuticals, including the enactment of the Medicines Act of 1968, which delineated specific parameters for the testing of drugs before they could be approved for use. However, the very demographic that propelled these safety measures—pregnant women—has often been excluded from clinical trials, not due to any intent to harm, but rather from a persistent fear of repercussions, as explained by Mariana Widmer, a maternal health scientist at the WHO. “People have been scared to treat pregnant women since the thalidomide tragedy,” she noted. “Pregnant women are scared to be treated.”
On that note, Widmer emphasises the need for collaboration among various stakeholders to effect change, acknowledging that “this is a huge process that will take time” and requires extensive partnership development. Current practices often leave healthcare providers in the position of explaining to pregnant patients the uncertain safety profiles of medications due to a lack of testing, leading to difficult conversations about the risks and benefits of treatment.
The World Health Organization indicates that maternal health cannot be sidelined; alongside preventable conditions, chronic diseases such as heart disorders, diabetes, and epilepsy remain significant contributors to maternal mortality rates worldwide. “Pregnant women are still dying from conditions that are otherwise preventable in others,” Widmer stated, underscoring the gravity of the situation.
Emma poignantly illustrates this dilemma through her experience with Nabilone, a drug used to manage her debilitating nausea and vomiting. “Before I had the [Nabilone], I was in hospital every few weeks needing IV replacements and electrolyte replacements. So it’s all being deemed safer that I stay on them because we know what’s going to happen if I don’t. And that’s probably more dangerous,” she explained. The absence of randomised control trials raises questions regarding the risks of medication usage during pregnancy, particularly with substances derived from cannabis, as much of the information is extrapolated from data involving recreational users, complicating the decision-making process further.
The WHO plans to assess essential medications for prevalent chronic diseases and develop guidelines to ensure that future drug tests incorporate pregnant women where feasible. By incentivising pharmaceutical companies to prioritise this research, the WHO hopes to encourage faster drug approval processes post-testing.
Reflecting on past lessons, Prof. Widmer assured that advances in science enhance our capacity to safely conduct clinical trials. “We have the means to know how to do it properly in order to ensure that the woman is safe and that the baby is safe,” she affirmed, outlining a structured approach beginning with laboratory studies before progressing to trials involving non-pregnant individuals and those with health conditions.
Dr Teesta Dey, an NHS veteran turned global health consultant, shared her own maternal journey as further motivation for advocating change in this area. Following a complicated pregnancy, she recognised the confusion surrounding medication safety, leveraging her experiences to address these systemic gaps. “That left me in a real quandary because I didn’t know, could I use it? Is it safe for me? Is it safe for my baby?” she remarked, highlighting a lack of transparent information that resonates throughout maternity care.
The ongoing dialogue around drug safety is crucial, particularly given the complexities revealed during the Covid-19 pandemic, where many vaccine studies excluded pregnant women. Even with subsequent data affirming safety for pregnant populations, the initial omission fostered a climate of mistrust. Dr. Dey noted, “Yet they didn’t include them in the study,” pointing out disparities in care that continue to have ramifications today.
As we navigate these intricacies of maternal health, the conversation is shifting towards a model encouraging the involvement of pregnant women, allowing them to weigh their treatment options. A WHO toolkit designed for both healthcare professionals and patients is anticipated this spring, aiming to foster safe and informed discussions. Dr. Dey firmly asserted, “Pregnant women are capable of understanding the risks and making the decision whether to take part in a trial for themselves,” a sentiment echoed by Emma, who expressed her willingness to participate in such initiatives if provided the opportunity.
In summary, the conversation surrounding drug development and pregnancy is ripe for transformation, reflecting a fundamental shift towards recognising the autonomy and needs of women in their healthcare decisions. As the global health community mobilises towards this goal, there is hope for more informed choices in the future, ensuring that the lessons of the past do not repeat themselves and that women are no longer sidelined in discussions concerning their health.
Our Thoughts
The article highlights the ongoing challenges faced by pregnant women regarding medication safety, emphasizing a significant gap in clinical trials for this population. To prevent similar incidents, regulatory bodies must ensure that pregnant women are included in drug testing phases, aligning with the UK Medicines Act 1968, which mandates rigorous safety assessments before medications are administered. The exclusion of pregnant women from trials perpetuates uncertainty about medication safety and undermines their health, potentially breaching the Health and Safety at Work Act 1974, which obliges employers to ensure the health and safety of all workers, including expectant mothers.
The lessons learned stress the importance of balanced risk assessments that consider both the risks of untreated chronic conditions and the potential harm from untested medications. Collaborations among health authorities, pharmaceutical companies, and insurers are crucial to establish clear guidelines for safely including pregnant women in trials. Implementing these changes can empower women to make informed decisions about their healthcare without fear or guilt, improving maternal and fetal health outcomes in future.